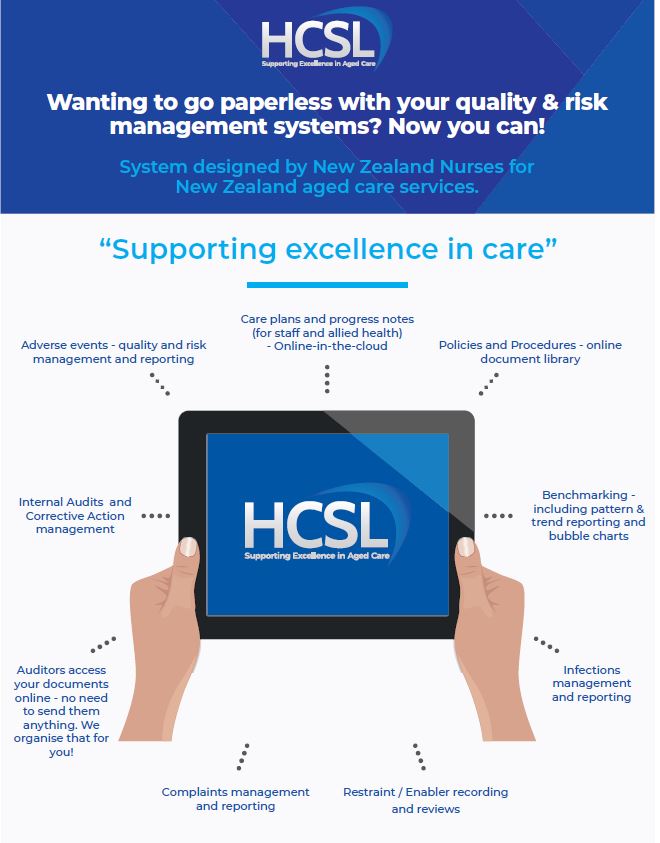
HCSL Aged Care Software incorporates quality and risk, bench-marking, internal audit management systems as well as clinical functions) and how to use them. These systems have all been audited numerous times for ARC provider Certification with maximum four year outcomes being achieved where the system is fully implemented. Tried and testing; pre-approved audit compliant.
Please click on the following links (the blue words below) to watch videos which describe the functions of the HCSL Aged Care cloud-based aged care software.
Gives you a general over-view of the key Dashboard and Resident clinical management functions available as at December 2019.
Guides you in how to upload or change a resident photo within their online profile
Guides you in how to add, view or search resident progress notes.
The HCSL system functions are able to be used in their entirety or some care providers use only the policies and procedures with the dashboard for quality and risk management; while others use the full system including the care planning and progress notes.
We have several care provider sites currently who have become paperless using the HCSL system in conjunction with Time-target, Medimap or 1chart and InterRai. The mix of paper based and IT based depends on your site, the IT skills of your staff and their access to computers. There are a range of service options available depending on what suits your current circumstances. To find out more about the service level options available click here
We continue to add features to evolve the system in response to changes in clients and industry needs. This evolution is intended to be an ongoing process and we look forward to your feedback and ideas. Each change is considered on the basis of how it can be used by clients to ease their workload, streamline and save time while giving useful information.
HCSL Aged Care software systems are created by Healthcare Compliance Solutions Ltd through Version 1 or for version 2. Access codes are provided to clients with a current service agreement in place.
If you would like more information on the services which are available click here.
If you would like to receive our HCSL Aged Care newsletter which is published every 6-8 weeks, email us on gill@agedcarecompliance.com with your contact details. This is also the email address if you have any further questions on HCSL software and services.