Posts
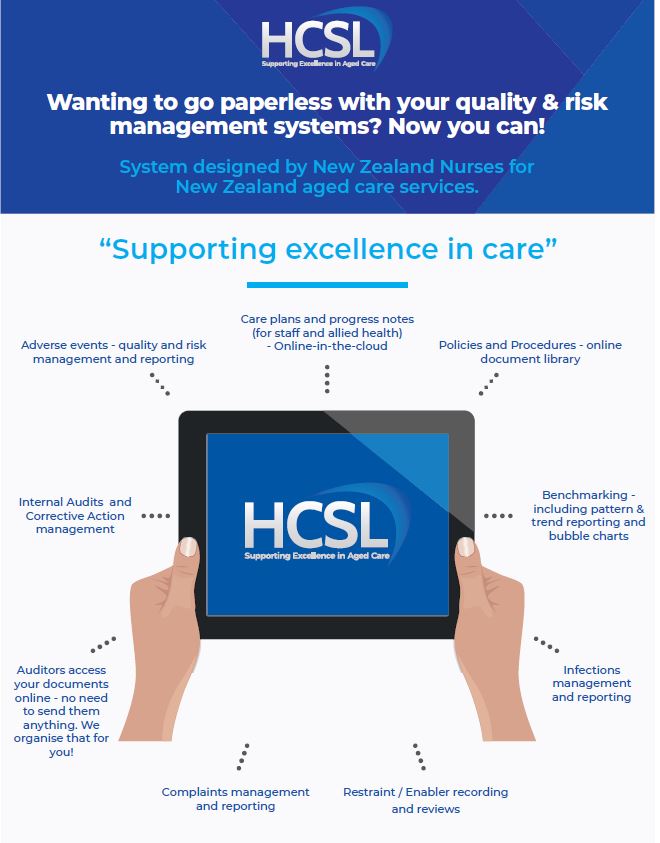
HCSL Aged Care Software incorporates quality and risk, bench-marking, internal audit management systems as well as clinical functions) and how to use them. These systems have all been audited numerous times for ARC provider Certification with maximum four year outcomes being achieved where the system is fully implemented. Tried and testing; pre-approved audit compliant.
Please click on the following links (the blue words below) to watch videos which describe the functions of the HCSL Aged Care cloud-based aged care software.
Gives you a general over-view of the key Dashboard and Resident clinical management functions available as at December 2019.
Guides you in how to upload or change a resident photo within their online profile
Guides you in how to add, view or search resident progress notes.
The HCSL system functions are able to be used in their entirety or some care providers use only the policies and procedures with the dashboard for quality and risk management; while others use the full system including the care planning and progress notes.
We have several care provider sites currently who have become paperless using the HCSL system in conjunction with Time-target, Medimap or 1chart and InterRai. The mix of paper based and IT based depends on your site, the IT skills of your staff and their access to computers. There are a range of service options available depending on what suits your current circumstances. To find out more about the service level options available click here
We continue to add features to evolve the system in response to changes in clients and industry needs. This evolution is intended to be an ongoing process and we look forward to your feedback and ideas. Each change is considered on the basis of how it can be used by clients to ease their workload, streamline and save time while giving useful information.
HCSL Aged Care software systems are created by Healthcare Compliance Solutions Ltd through Version 1 or for version 2. Access codes are provided to clients with a current service agreement in place.
If you would like more information on the services which are available click here.
If you would like to receive our HCSL Aged Care newsletter which is published every 6-8 weeks, email us on gill@agedcarecompliance.com with your contact details. This is also the email address if you have any further questions on HCSL software and services.
I was first introduced to Gillian Robinson of Healthcare Compliance Solutions Ltd (HCSL) in 2016 when I took up the Facility Manager position at Terrace View Retirement Village.
The facility had HCSL in place but were not fully utilising Healthcare Compliance Solutions policies. The first thing to do was to get Terrace View fully operational under Healthcare Compliance Solutions. Gillian was very supportive during this change providing education to myself, Clinical care manager and our team.
HCSL aged care software is easy to find your way around. Our Nurses have reported that care planning in HCSL is saving them time. Everything is in a logical order.
Features that make my role easier are the ability to track trends in adverse events and infection control. To be able to bench-mark our data within the industry to see how we are trending against our peers.
Terrace View is very excited to be moving to HCSL aged care software version 2 so we can become fully electronic. To be able to search a file or document from the computer saves all the team time.
Gillian’s knowledge of the aged care industry and how the sector works is reflected in the software she has developed and is designed to increase nursing team efficiency in a very time restricted environment.
Donna Coxshall
Facility Manager
18th February 2020
We are very pleased to have recently been granted 4 year MOH Certification! No corrective actions and three Continuous Improvements.
This follows on from a fully attained Partial Provisional Audit that was required prior to opening our two new wings earlier this year with no corrective actions.
Make no mistake! HCSL policies, software and support have played a major part in these accomplishments. The HCSL software we use means we have easy access to information in real time.
I started working with Gillian of HCSL shortly after I took on the role of Facility Nurse Manager at Bethsaida Retirement Village six years ago. The facility was not using Healthcare Compliance Solutions policies at the time and perhaps this was reflected in the previous audit results.
Gillian is always responsive to emails and phone calls which is critical when timely advice is required.
The HCSL regular newsletters are interesting with relevant and up to date information on issues affecting aged care.
Gillian is a lovely person to deal with. She is thoughtful, professional, pragmatic and I have always found her to be keen to help, with practical advice on any issues that might arise in the management of a retirement facility.
I thoroughly recommend HCSL to all aged care facilities.
Tracy Holdaway RN BN
Facility Nurse Manager
Bethsaida Retirement Village
August 2019
The question of whether mandated minimum nursing hours would work has been asked previously. The workload of care and nursing staff is frequently discussed with staff reporting they are pressured for time to complete all the necessary duties assigned. The Nursing staff have different but over-lapping functions to care staff. When reviewing your staffing, it’s important to include a number of factors into any review when looking at the productivity and efficiency of your team.
We suggest you look at not only leadership and skill-mix, which are vital for safe services but also consider other factors. These can include the location of high acuity needs residents within your service. With an increase in the use of dual beds, the mix between rest home and higher acuity hospital level of care are now intermingled and not specifically allocated to one area of the building. This means the Registered Nurses providing clinical monitoring and oversight may have to spread their attention to a much more fragmented and broader geographical area in your service than was previously the case.
The location of resources and time spent looking for items of use and equipment could be minimised if more thought was put into the design of new facilities and the locating and management of replenishing stores for ready access by staff as and where they need them. Who does the running and fetching could also be considered in work roles so staff with high end clinical skills are spending the bulk of their time on performing functions specific to their role and skill. Not doing tasks that could be better delegated to others.
After the recent sudden closure of a care facility in Australia without apparent planning or communication with families, there has been outrage that such a thing could happen. The “Queensland Premier Annastacia Palaszczuk announced her Government would order fixed nurse-to-resident ratios in state-owned aged-care facilities.” The ABC news report (19th July 2019) goes on to say “at least 50 per cent of staff having contact with residents in 16 publicly run aged-care centres to be nurses.” I don’t know if by nurses they mean Registered Nurses only and not Enrolled nurses but I can’t help wonder if this alone will ensure safety.
One year on from Simon Wallace (NZACA CEO) reporting on staffing shortages, we haven’t seen any improvement it would seem! In New Zealand an increasing proportion of our Registered Nurses have come to New Zealand to practice with no prior working knowledge of aged care services. They frequently have limited aged care related experience to conduct the complex assessment and clinical management of high acuity residents in a residential care setting. This is not to diminish their value as we can’t provide the services needed otherwise.
What I’m trying to highlight in the current circumstances is, we’re frequently seeing nurses set up to fail or provide less than safe care as they simply don’t have the experience in this specialised field of nursing. I recall conversations in the early 1990’s predicting a massive nursing shortage. It appears that in the time-span between then and now, we haven’t addressed this issue.
We welcome comments and suggestions of how this could be addressed here in New Zealand before we end up in the depths of a staffing crisis which halts care.
Hi Gillian
Just passed our two day audit – NO NON COMPLIANCES; NO PARTIAL COMPLIANCES !!!!!!!!!!!!!!!! – thank you so much for your efforts.
The auditor praised your system – said it was a really good system – met all the requirements of the standards, is written in plain language, all the documentation relating to my job ie quality, risk management is outstanding and more than meets the standards and is very well used in the context it should be – thanks!
Lois Lash
Quality Assurance
Ascot House – Tainui Village
Testimonial – Chatswood Resthome and Hospital owner (and Clinical Advisor for NZ Aged Care Association)
I am very happy to endorse your system as the information is invaluable for CNMs to analyse the data/information and make informed decisions on best practice and innovation to decrease hazards, improve outcomes, and mitigating factors for resident welfare. I’m pleased you are delving into the data to the level you are, as it’s time saving for sites in many respects, and so easy to dice and slice the information to get the trends.
CNM’s used to spend hours just writing up the collective information before the analysis, so this system is hugely time saving.
Rhonda Sherriff
Chatswood Resthome and Hospital
(Clinical Advisor for NZ Aged Care Association)

Culture is a word we hear a lot and goes hand in hand with the concept of culture change. In this article I’d like to touch on how to facilitate culture change and why it is beneficial to your long term care setting. Let’s face it, aged residential care in New Zealand is changing rapidly and this impacts the experience of residents, staff and visitors to long term care settings. It impacts their desire to be in your care facility or to move somewhere else. This applies to be both residents and staff. Families often choose the care provider for their elderly relatives. What do they perceive when they visit you?
There are also barriers and challenges to creating and sustaining a definable and deliberate culture. The experience of the residents and staff is a result of the culture (behaviours) which should be aligned to your organisation values, mission and goals. There are well publicised workforce shortages and high turnover of staff. Long term care is also in the middle of change from paper-based systems to electronic storage and management of information. The environment in which care is being provided is also changing through new construction of buildings from a institution to non-institutional. The atmosphere being created by those within the long term aged care residential setting is changing to a more relaxed feel.
Nursing care and direct support is now also being provided within retirement village studios, apartments, villas, homes. This means a change of not only the context of care. Ensuring person centred care where each individual feels seen, heard and respected takes consistent focus and strong leadership. Not always easy in a industry that is changing in so many ways. I wrote in a previous article on workplace culture that behaviours could be a better point of focus rather than simply focusing conversation on culture as a concept.

The behaviours which support a culture you can be proud of and one that sets you as an industry leader, require a long term focus and not just a one time exercise. The strong leadership needed along with education and ongoing communication is key to setting a desirable culture. Have you aligned your staff, management and Governance behaviours with your organisation vision and mission statements? Behaviours reflect actions and they can be optimal actions, good actions, poor actions or non-action. All will have an outcome which impacts the residents experience and determine how they feel about residing in your long term aged residential care setting.
For change to occur there needs to be a focus on improvement, a reason to change which residents and their families see as beneficial. We tend to stick to doing what we’ve always done unless we can see a personal gain or something which provides a sense of satisfaction on a personal level. What’s in it for me? Culture change is not something that’s going to be achieved from a top-down approach. It’s going to take engagement from all levels of the organisation and create wins for those involved. Without perceived gains or wins, people stay stuck in old habits which don’t fit the new expectations of those seeking care and support.
If you’re the manager or CEO and delegate a ‘change management’ process to someone else, then expect to check in later to find wonderful results without your direct involvement and engagement, you may be disappointed. Culture change is a team effort. To achieve change, everyone needs to participate. They need to believe in the outcomes you’re trying to achieve with whatever strategies or initiatives you put in place.
Who is going to lead change? There is an old saying that everything flows from the top down and this is also true of culture. If the Board are dysfunctional then there should be no surprise when staff working at all levels of the organisation are dysfunctional. How is communication about strategies of change being done to gain buy-in? How are you going to measure your change initiatives to find out if you’ve been successful? How are you going to ensure the desired culture is maintained? There are a number of tools (mostly overseas based) which can be used to start this process. Here is a free online culture change assessment tool you could use.
What is the experience of your resident and your staff on a daily basis? Would they recommend you to others in a way to reflects loyalty to your care facility as a preferred place to live or work? If not, what are you going to do about it?
ONE EXPERIENCE OF NOROVIRUS MANAGEMENT
Some may think the actions a little extreme but the objective was to minimise risk to others and in doing so, minimise the numbers of people (residents and staff) infected with Norovirus. The below is how one facility dealt with a norovirus outbreak recently.
Here’s how we dealt with what happened in our facility:
With the Clinical Nurse Manager on annual leave at 8.00 am on Friday 11 January the Senior RN advised the QA we had two suspected cases of vomiting and diarrhoea. At 10.00 am the Senior RN advised the QA we could have four more cases of diarrhoea.
An immediate meeting was called with management and the situation discussed. The following steps were instigated –
- We immediately referred to our HCSL Safe and Appropriate Infection Control policy manual.
- We decided to take the “worst case” scenario approach eg Norovirus.
- We then set out an “action plan” and held a meeting at 11.00 am with all the staff present to advise the situation and actions to be taken –
Action Plan
- Infection Control at DHB were advised and samples were sent for analysis
- The Rest Home was put into “lock down”. The families and next of kin of all the residents were advised.
- The Village residents were advised and instructions given to them on procedures to follow.
- The doors between the three sections of the Rest Home were closed and staff confined to these areas only – no exceptions.
- The infection log from HCSL system was immediately put into use – an RN had to sight all vomit and diarrhoea together with noting the times and dates – this information was supplied on a daily basis to DHB – this information was imperative to identify if virus was spreading, how quickly, or if it had been confined to certain areas etc.
- The RNs appointed “dirty” nurses on each shift. A “clean” person was also appointed for delivering supplies around the whole rest home. Trollies were meticulously sanitised when “travelling” between these areas.
- Kitchen staff were confined to the kitchen only
- All residents were confined to their rooms with meals being delivered using “clean” and “dirty” trollies. This may seem extreme but the residents were agreeable to this.
- Diagrams out of our policy manual were put in the Nurses Stations on how to put on PPE. Full PPE was mandatory in all “dirty” residents rooms and when serving food or drinks. Face masks were mandatory for all staff at all times – no exceptions. Full face shields were used in the laundry and any very soiled linen was disposed of as per instructions.
- Hand washing and sanitising techniques were vigorously adhered to.
- The cleaners were issued with “heavy duty” cleaning products and all vacuuming was banned.
- Being an older Rest Home with only certain areas being air conditioned it was easy to turn off all conditioning and keep off.
- Residents were encouraged to open their windows for fresh air and let in the sunlight.
- Cleaning equipment was kept in the “dirty” rooms for their use.
- All residents were advised to put toilet seats down prior to flushing and flush twice.
- All residents and staff were reminded of hand hygiene practices and we ensured the appropriate supplies of hand washing and hand hygiene gels were available.
- Communal areas in the Rest Home were closed, cleaned, sanitised and not used.
- Management held a daily meeting at 9:00am to report on the up to date situation and a report was issued to the staff at 1:00pm and a daily report issued to the DHB.
- The rest home was advised by DHB ON 16 January 2019 to let residents out of their rooms but stay confined to the areas of the Rest Home they lived in
- On 21 January 2019 the rest home underwent a complete steam clean of carpets, drapes etc,
- On 22 January 2019 we re-opened the Rest Home to visitors again.
LESSONS LEARNT
We had a total of only 4 confirmed cases of Norovirus – one in the hospital and three in the rest home. At the time the Rest Home was fully occupied (60 residents).
Follow your Policies and Procedures “to the letter”. Without the excellent information contained in our policy manual we would not have achieved the result we did as everyone had varying views on what to do. We had only one “view”.
We received congratulations from our DHB on handling this situation and receiving the outcome we did.
And of course we knew we always had the back-up of Gillian at HCSL either via email or telephone if required.
Hi Gillian,
Great news, we did very well with the audit.
The Lead Auditor tells us she cannot see we have any corrective actions to complete!
Also she acknowledged a CI from one of the Quality Improvements I completed. She was very impressed with the Quality and risk management systems via your Policies and procedures and says we are using your systems to the max.
Well, where would we be without your Policy and Procedures, they are great to work with – thank you.
kind regards
Rose Kennedy (Dixon House – Greymouth)
Contact Info
+ 027 601 6400 (Director)